Alzheimer’s Disease: Understanding and Managing the Journey
Kay
- 0
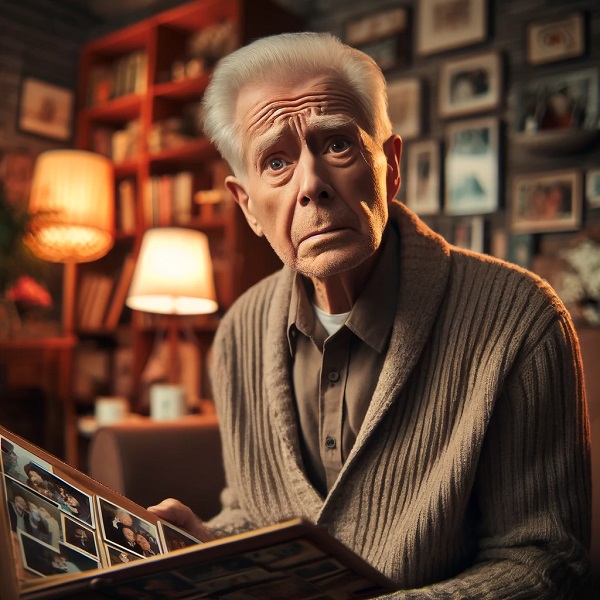
Alzheimer’s disease is known as the long goodbye. Seen as the definitive dementia, it slowly erases memories and abilities, altering the very way someone lives. In this article, we discuss what Alzheimer’s is, its symptoms, causes, and also how to manage it.
What is Alzheimer’s Disease?
Alzheimer’s disease is an irreversible, often fatal disease that destroys memory and other important mental functions. It is the most common cause of dementia, a facility that affects memory, thinking, and language, which in turn impacts independence and quality of life. Approximately one in 10 people over the age of 65, and almost half of those over 85, have Alzheimer’s dementia. Currently, it is thought to affect more than 5 million Americans. This disease devastates the brain by destroying brain cells. It typically begins by eating away at short-term memory, eventually causing memory loss and a decline in most of an individual’s intellectual abilities.
The History of Alzheimer’s Disease
Courtesy the National Library of Medicine, USA Alzheimer’s disease was first described by the German neurologist Alois Alzheimer in 1906. He studied the autopsy of 55-year-old Frau Auguste Deter who had died after suffering severe memory loss, language problems and a tendency to bellow out erratic demands. On close examination of her brain, Alzheimer discovered that it was dotted with a high number of abnormal clumps (amyloid plaques) and tangled bundles of fibres (neurofibrillary tangles) that he believed should not have been there.
Symptoms of Alzheimer’s Disease
Alzheimer’s symptoms manifest gradually and worsen over time. They interrupt your daily life and compromise your independence.
Early Symptoms
Some of the earliest warning signs are memory issues (such as forgetting words or names, or having difficulty performing familiar tasks); trouble with accessing or retrieving words; difficulty with spatial navigation – even getting lost in one’s own neighborhood; and physical difficulties, such as constant fumbling with things.
Moderate Symptoms
As the disease progresses, your loved one might become increasingly confused, moody and display behavioral differences. He might no longer recognize his family or friends; he’ll experience greater memory loss and need assistance with daily tasks.
Severe Symptoms
In the late stages, they can no longer speak, need round-the-clock care for daily care, and develop severe physical problems. They might become bedridden and lose their ability to swallow.
Causes and Risk Factors
Their cause is unclear, but some, like Alzheimer’s, appear to have complex risk factors that could trigger them.
Genetic Factors
Genetics is important. People with a family history of Alzheimer’s have a higher risk. Some genes, such as APOE-e4, increase the risk as well.
Lifestyle Factors
Lifestyle choices are among the factors that influence risk, with diet, exercise and cognitive engagement being particularly important. Smoking, obesity and lack of physical activity are strong risk factors.
Diagnosis of Alzheimer’s Disease
It is important to note that diagnosing Alzheimer’s disease is a complex journey that not only involves examining symptoms but also a lengthy and in-depth evaluation by a practitioner. That being said, here is a thorough portrayal of all the steps and techniques used to arrive at this diagnosis.
Medical History and Physical Exam
The first step in diagnosing Alzheimer’s is collecting a detailed medical history and conducting a physical exam, which assesses a person’s overall health and identifies symptoms associated with the disease.
Medical History review: The clinician will ask about the patient’s medical history (including past illnesses, medications taken and family history of Alzheimer’s or late-onset illnesses), as well as recent behavioral and personality changes and history of cognitive symptoms.
Physical Exam: This permits a thorough physical examination to exclude other potential conditions that might produce the same symptoms. For example, he will take blood pressure and heart rate to determine if there are any underlying diseases. He will then do a general physical examination.
Neurological Exams
Neurological exams are a great way to make sure your nervous system is working in the right way and identify any red flags.
Cognitive Tests: These assess aspects of cognition such as memory, problem-solving skills, ability to pay attention, language functions and other domains. Well-known cognitive tests include the Mini-Mental State Examination (MMSE) and the Montreal Cognitive Assessment (MoCA).
Sensory and Motor Function Tests: Tests of balance, coordination, reflexes and sensory response, which determine if there are neurological problems that might be causing the symptoms.
Brain Imaging
Brain imaging is also used to see the structure of the brain and whether or not it has abnormalities that could be related to Alzheimer’s disease.
Magnetic Resonance Imaging (MRI): In an MRI scan, a patient is placed inside a magnetic field, and radio waves enable the acquisition of an image of the brain’s anatomy. An MRI scan can reveal shrinkage of the brain, which can indicate dementia. In addition, these scans might also rule out abnormalities such as strokes and tumors that could cause similar symptoms.
Computed Tomography (CT) Scan: CT scans create cross-section pictures of the brain. They can detect atrophy of the brain as well as other structural changes related to Alzheimer’s.
Positron Emission Tomography (PET) Scan: PET scans detect amyloid plaques, the hallmark of Alzheimer’s disease. A tracer containing radioactive dye is injected into the circulatory system, which lights up areas of amyloid build-up in the brain.
Laboratory Tests
Laboratory tests are performed to rule out other potential causes of dementia-like symptoms.
Blood Tests: Blood tests can identify vitamin deficiencies, thyroid problems or infections that might occur together with cognitive problems.
Lumbar Puncture (Spinal Tap) : When this is done a cerebrospinal fluid (CSF) sample can be obtained and specific biomarkers – beta-amyloid and tau proteins – can be studied.
Genetic Testing
Particular genes linked to a high chance of getting Alzheimer’s can be identified with the aid of genetic testing.
Presence of APOE-e4 Gene: Carrying at least one copy of the APOE-e4 gene puts one at higher risk of Alzheimer’s. Yet not everyone with the APOE-e4 gene gets Alzheimer’s. Likewise, not everyone with the disease has this gene.
Other genetic mutations: Identifiable mutations in the genes APP, PSEN1 and PSEN2 are not that common, and account for fewer than 1 per cent of cases in people with early-onset Alzheimer’s. When these mutations are identified, patients and their families are usually referred to a genetic counsellor to discuss what the results mean.
Psychiatric Evaluation
A psychiatric evaluation can also be used to rule out psychiatric conditions such as depression or anxiety that can mimic, or potentially contribute to, Alzheimer’s symptoms.
Mental Health Assessment: Interviews and questionnaires to assess mood, behavior and psychological health. The interview helps to determine whether any other psychiatric conditions are present.
Combining Diagnostic Information
Instead, a diagnosis of AD is typically based on all of the above tests, among others, so that providers can make a ‘best guess’ and offer an appropriate treatment plan.
Differential Diagnosis: Since Alzheimer’s dementia can be distinguished from other types of dementia (including vascular dementia, Lewy body dementia and frontotemporal dementia), the treatment approaches can also vary.
Continuous Monitoring: Since Alzheimer’s is a disease that FOLLOWS a linear progression, continuous monitoring and follow-up evaluations are required to adapt to the changing care plan as the dementia progresses.
Dementia due to Alzheimer’s
This phase includes mild, moderate and severe dementia, with increasingly severe symptoms and impaired cognition and functional capacity, and a progressive need for assistance from others with activities of daily living.
Treatment and Management
While there’s no cure for Alzheimer’s, treatments can help manage symptoms.
Medications
Certain drugs can slow down memory loss and improve quality of life for a period of time. These include cholinesterase inhibitors and memantine, which are prescribed treatment options.
Non-Drug Approaches
Cognitive therapies, physical activity and social engagement can boost mood and preserve cognitive reserve.
Supportive Care
Caring play an important role in offering support and care, which includes clear structure, safety and emotional support.
Living with Alzheimer’s Disease
Daily Life Tips
This includes doing things to stick to a routine, keeping tasks as simple as possible, using memory aids, and exercising.
Caregiver Support
Caregivers need care, too: respite care, support groups, and counselling can be helpful.
Research and Future Directions
We work toward better treatments, and a possible cure, with studies that are underway now. Genetic, brain-imaging and biomarker research are promising for the future.
Myths and Misconceptions
Stigma and fear often arise due to incorrect interpretations of Alzheimer’s. When common misconceptions such as ‘Alzheimer’s is just part of growing old’ or ‘Alzheimer’s only happens to the aged’ are spread, it becomes more difficult for those living with the disease to receive appropriate care, attention and support.
The Impact on Families
Alzheimer’s affects everyone. Emotional, financial and physical stress can arise and family support and resources can make all the difference.
Community and Resources
Many, many resources are also available to help patients and their families – from local support groups to local or national drug-awareness charities to online support communities.
Conclusion
But, armed with knowledge, community support, and people, places and things that provide comfort and lower anxiety, life with Alzheimer’s can be better managed. Learn more; seek support; keep up with research as it becomes available – these are the ways we can take control of our lives and the lives of our loved ones with Alzheimer’s.
FAQs
Is there a way to prevent Alzheimer’s disease?
Although it’s not possible to guarantee that you will never get it, by keeping a healthy lifestyle, such as taking regular exercise, eating a balanced diet, keeping mentally active by reading or by playing board games with family or friends, stopping smoking and cutting down alcohol consumption, you can reduce your risk of developing it.
Which of the following are early symptoms of Alzheimer’s?
Paraphrased: Memory loss; difficulty performing familiar tasks; problems with language; disorientation to time or place; changes in mood or personality; loss of initiative.
When is Alzheimer’s disease detected?
It’s diagnosed by medical history, physical and neurological examination, cognitive tests and brain imaging.
Is there a cure for Alzheimer’s disease?
There isn’t anything that can stop the disease at this time, but there are medications and non-drug approaches that can reduce symptoms and help patients live well with the disease.
How to help someone with this disease who still lives at home as an Alzheimer’s caregiver
Must: maintain routines; simplify tasks; offer reassurance; and get respite care and support groups.
LG V60 ThinQ Samsung Galaxy A51 LG G8 ThinQ LG G8 ThinQ LG G8 ThinQ LG Velvet Samsung Galaxy S21 iPhone XR iPhone 12 Pro Max iPhone XR


